
Can Training in Extreme Cold Permanently Hurt Your Lungs?
Reviewed by Jason Koop,
Head Coach of CTS Ultrarunning
You’re right, you’re not going to “freeze your lungs”… however, exercising and competing in extreme environmental conditions can have a long lasting negative impact on your lung health. Every winter runners, cyclists, and triathletes flood social media feed covered in various forms of human icicles, temperatures flash across the screen “0F” “-16F” “-36F”, wind chills dropping the skin temperature lower. Every winter athletes and coaches cringe and have to ask, “at what cost?” Is there a specific purpose to be gained, aside from “proving your own toughness”, by slogging out the miles as temperatures dip below zero?
Of course, you may live in a cold, wintery place and you train outdoors on a regular basis. Perhaps you participate in cross-country skiing, ski mountaineering, or other high-intensity winter activities. As coaches, we receive questions from athletes about the potential risks of training in extreme cold. The short answer is, yes, there is an increased risk for developing a hyper-reactive airway, or what is now called exercise induced bronchospasm (EIB), what was originally called exercised induced asthma.
Exercise Induced Bronchospasm
Think of EIB as an overuse injury of the lungs. The cells that line your lungs are incredible, and they have an amazing capacity to repair themselves quickly. However, this repeated injury-repair cycle is responsible for adaption and structural change that is not always positive.
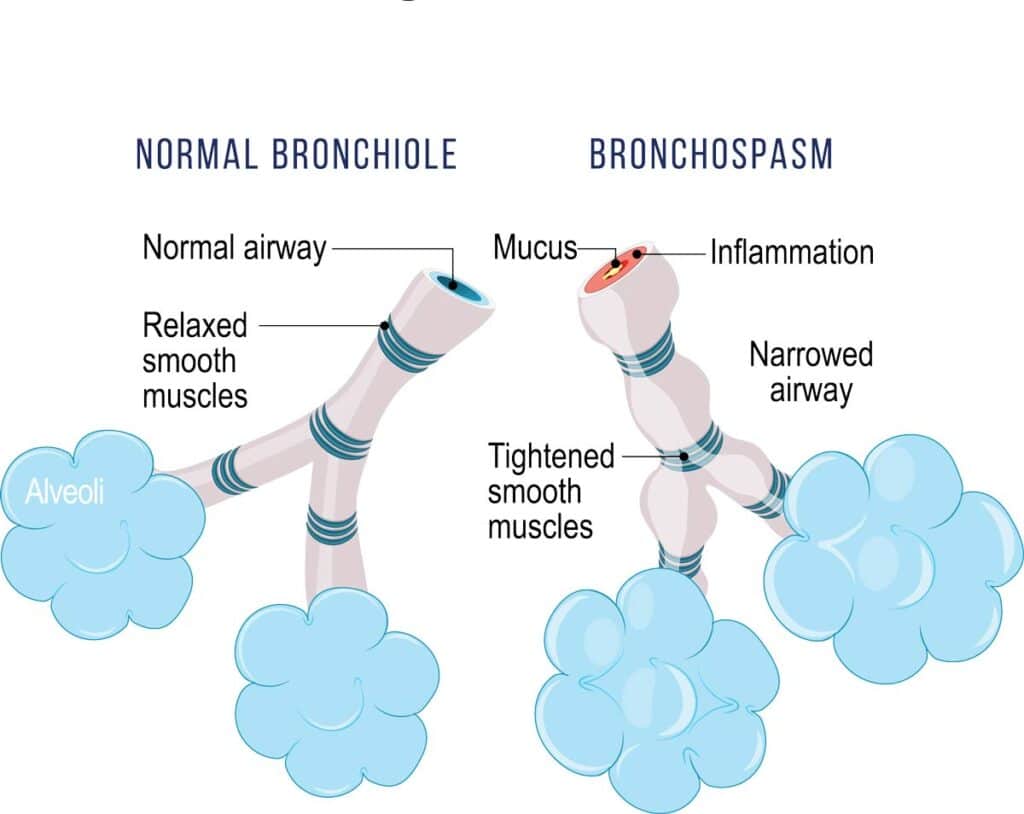
When you exercise your ventilation rate increases, and when combined with another variable like cold and/or dry air (note that the issue with extremely cold air is that it is extremely dry), you cause water to evaporate from the airway surface liquid that makes up the lining of your bronchioles at a rate your body cannot keep up with. This drying causes a shift in the osmotic gradient, or the movement of liquid, of the cells lining your airway, which stimulates the release of inflammatory mediators. These inflammatory mediators, like histamine, can influence the smooth muscles of the bronchioles, causing constriction, mucus build-up, and edema (swelling) (1).
Now, this is a slow and progressive problem. One day of training in extreme cold does not guarantee a lifetime of breathing issues. However, continued training in extreme environments does heighten your risk. There are certainly factors that may predispose you for developing EIB, including; high intensity activities, history of asthma, allergies, a history of atopy (or being hyperallergric, and allergic rhinitis (an allergic reaction to airborne allergens) (5). Additionally, the environmental conditions you regularly train and race in are known risk factors, including cold air, dry air, high pollen counts, pollution, insecticides, fertilizers, wildfire smoke, chlorination, car exhaust, etc (5).
Risks Over Time
As mentioned above, this airway inflammation and airway limitation appear to progressively worsen over a season and over a lifetime in many endurance athletes, with 90% of the asthmatic population and 20% of the general population reportedly developing EIB (1,2, 5). You might be thinking to yourself, so that one training session is probably okay, and honestly you might be right. However, what we gathered in the lab on skiers was that even after a single week of training or racing in single digit temperatures all of the skiers in the study suffered a varying decrease in measures of expiratory volume (amount of air you can forcefully exhale), which could translate to a decrease in performance.
That’s right, if not for your general health, do it for your performance. The demands we place on our pulmonary system as endurance athletes is immense, sometimes so much so that we exceed the capacity of that system. The repeated drying of your airway surfaces over time can cause a thickening of those membranes (2). This causes a reduction in our ability to combat the evaporation of the liquid surface of our airways (1) so that your airways become more sensitive to irritants over time. This makes EIB progressive in nature, and ultimately leads to a ventilatory limitation during performance as a result of those permanent airway-structure changes due to frequent environmental exposure (3,4).
► Free Cycling Training Assessment Quiz
Take our free 2-minute quiz to discover how effective your training is and get recommendations for how you can improve.
Protecting Your Lungs
So what can you do to protect your lungs?
Move your intervals inside.
If you can avoid doing intervals outside when the temperatures dip into the single digits, do so. It’s not so much the running that is the issue but the increased breathing rate during intervals that can cause the problem. It’s for that very reasons that the international ski federations do not allow races to take place if temperatures are below -4F to try to limit exposure of the athletes. Think of this as improving the quality of the work you are able to do.
Invest in a mask.
A Buff will not do. A Buff is great at protecting your skin from cold air, wind, and sun exposure. What it cannot do is effectively warm the air you are inhaling. There are relatively affordable masks designed exactly for the purpose of training and racing in extreme cold. AirTrim, made popular by Scandinavian skiers, is a great product.
Shorten the total duration.
Part of the lung equation is a combination of how hard you are working and how long you are working. Along with moving the hard work inside when the temperatures dip below zero, think about shortening your total workout length. Cold exposure is harder on your body metabolically (you have to stay warm after all) and so your typical run will have a higher stress load on your system.
References
- Rundell, K., & Jenkinson, D. (2002). Exercise-induced Bronchospasm in the Elite Athlete. Sports Medicine, 583-600.
- Kippelen, P., Fitch, K., Anderson, S., Bougault, V., Boulet, L., Rundell, K., Malcolm, S., & Mckenzie, D. (2012). Respiratory health of elite athletes- preventing airway injury: A critical review. British Journal of Sports Medicine, 471-476.
- Sheel, A., Macnutt, M., & Querido, J. (2010). The pulmonary system during exercise in hypoxia and the cold. Experimental Physiology, 422-430.
- Boulet, L. (2012). Cough and upper airway disorders in elite athletes a critical review. British Journal of Sports Medicine, 46(4), 417-21.
- Molis, M. A., & Molis, W. E. (2010). Exercise-Induced Bronchospasm.Sports Health: A Multidisciplinary Approach,2(4), 311-317. doi:10.1177/1941738110373735
► FREE Mini-Course: Learn How to Maximize Your Limited Training Time
Learn step-by-step how to overcome limited training time and get faster. Walk away with a personalized plan to increase your performance.

Comments 27
Thank you Dr. Dennis.
This is a great article. A few years ago (I teach high school and dual credit chemistry) one of my students commented that my running outside was bad for my lungs. I decided right then and there to look up research to refute his claims.
He was right. And my breathing has greatly suffered (even though after that point I wore a buff – which your article points out isn’t enough). I’m not the fastest runner, but I had no problem mentally with going out in the negative (F) windchills and getting some distance now.
Now I’m basically allergic to life and while I haven’t been formally diagnosed with EIB, I now end up wheezing and having a hard time breathing when I merely laugh too much.
Don’t mess with your lungs.
Go see your doctor. There is treatment available and you can have your life back. EIB does not harm your lungs permanently, it just makes it harder for a while.
Fantastic article and something that has intrigued me over the years. I ran for 15 years and never stopped running no matter what the season. It was so cold I used to put vaseline on my face but never worried about the cold air I was breathing in. (Alberta, Canada). However, what has happened to my lungs over this period is to have highly sensitive airways and I have repeatedly gotten bronchial infections and pneumonia twice. I blame this all on my cold weather running.
Pingback: Exercise and Air Pollution: Training and Racing When Air Quality is Poor - CTS
I just ran outside in -5C for the first time since last summer about a week ago without covering my mouth, I didn’t know this could cause problems. Since then have had a cough and lung irritation and breathing issues. How long will this last?
Thank you for sharing. From my unfortunate experience…….. I ran ultra in the mountains (Zhejiang, China) and slept in the cold tent the night after. Soon, after returning to the city (Shanghai, China) I discovered difficulties with breathing. What became worth the week after. After seeing the doctor I ended up with an asthma diagnosis and corticosteroids and spray prescribed. It was just the beginning. To be frank, sometimes, in the days when pollution is high (which is not a surprise for Chinese cities), I was terrified not just to run outside but simply go out. After several months of therapy, I experienced a slight relief, but then I had a couple of terrible moments with acute breathing on cold and humid days. And, I had to find some alternative ways. What I found out was acupuncture. I don’t say it is a scientifically proven method but it worked for me to relieve the symptoms. Now, I am not taking any drugs. And living in a clear air environment (in Canada). However, I cannot go outside without a mask on the cold temperatures or when AQI is higher than 70.
I loved the scientific nature of this article. It is so much easier to follow advice when you understand the reasoning! One tiny point of contention though: I am guilty of venturing outside for a run or skate ski on cold Montana winter days but I attribute that more to the drudgery of indoor workouts than being an ego thing.
Thanks for the information, as it is very timely. I just had my annual checkup with my doctor and I told him I cough a lot when I exercise in the cold. He said I have exercise induced asthma. I can’t wait to tell him he used an outdated term and it’s called exercise induced bronchospasm (EIB). Fortunately, I have a great doctor and we have a very good relationship where we tease each other a lot 🙂 He prescribed an albuterol inhaler as a start to see if that helps.
You should ask whether your doctor thinks you need Singulair. It works great for EIB.
Interesting article especially since we are at 4 degrees in KC this morning with wind chill warnings. I’m 59 and as I’ve gotten older and spend more time on the trainer when it gets extremely cold. Getting soft I think! The past few years I’ve grown concerned in our area when we have the extreme heat and ozone alerts of summer mixed with our high humidity and almost no wind. Air quality becomes an issue on the road. My gravel bike has now become my go to weapon. I retreat to the trails and woods to be a little cooler (shaded) and to give my lungs hopefully a little break from the poor air. If you’ve done research on this flip side, it would be a very interesting read as well. Thanks!
great article, thanks! I am curious about the limits where the risk becomes higher when considering temperature, humidity and the type of exercise. Example, how about long endurance paced rides in temperatures near but above freezing? I’m sure it’s not something that is easy to answer quantitatively, but understanding those levers and how they drive risk up / down would be helpful in deciding how to train over the Winter months.
Now 74, I grew up in Fairbanks. I had a paper route which I delivered on foot. It took about 2 hours and temperatures were frequently -50 and below. If my feet started to freeze, I’d run. After one especially severe episode, I experienced what my mom thought was pneumonia, but which I now see as what’s described in this article. I also XC and Alpine skied there and then was on a XC ski team in college.
Yes, I have EIB and reduced performance, diagnosed as EIA, and treated with fluticasone and salmeterol, which works. Anyone with these symptoms should see a pulmonologist. Back when I lived in Fairbanks, my condition was called “frosting your lungs,” not uncommon.
I tried making my own air-heating face masks, but I was 12-14 and never made one that worked very well.
I do manage to perform well for my age, on the bike, skiing, and at high altitude. My medication has something to do with that.
Thank you as always for the free CTS education.
Best
Scott
Thanks for a great article! I live in Interior Alaska and spend my time outdoors cross country skiing and fat biking in winter. I’ve used the air trim masks which work great. However I’ve now switched to a different device called “Lung Plus.” This warms and humidifies the air and works quite effectively. As an added bonus it helps keep your glasses from fogging. If I don’t use it I’ll come in with a hoarse voice and a cough after a work out. When I use the lung plus I don’t get a cough or lose my voice.
So is there any consensus on what temps this becomes a potential or real problem? Single digits and lower or could it be teens and low 20’s even? I will routinely XC ski in single digit temps and below zero but absolutely just moderate effort. Exercise and enjoyment just being outdoors and usually just on weekends. Does this put one at risk.
It’s interesting since I always believed that world class XC skiers had some of the highest VO2 max levels on the planet (shame shame on Sports Illustrated for not including a world class XC skier in their fitest althletes. Total BS IMHO)
Pingback: 6 Steps to Take Time Off This Season Without Losing Your Running Base | The Runner's Trip: Run Long, Travel Far, Discover More
What a fascinating and informative article! I work with skiers of all kinds, so this is great information for me to pass along. Also explains why my husband, a lifelong skier and hockey player, starting getting cold induced breathing trouble in his 50’s. Thanks for a great read – I will share with my clients!
Very interesting! I never had issues until I moved from a tropical to a cold climate. Years after living in Chicago, I developed EIB and need to use an inhaler for high intensity excercise (indoors or out). And note that I never went outside un temps under 35-40F! My husband has it worse. He gets pneumonia every February unless he stays indoors all winter.
Thanks for this enlightening article Corrine.
I used to regularly climb 8k in 4 or 5 hrs. here in Palm Springs, Ca. almost weekly.
Most climbs were fine, but occasionally, I would literally feel like I was an out of shape mess.
Every little section that kicked up, brought me into a zone, (much lower threshold than normal), of almost gasping for air.
After much study, I thought it could be related to lack of hydration. I drink more than most, (usually close to a gallon on a climb like that), including electrolytes.
I’m wondering if 30 years of desert, dry-air training, (used to run some trail marathons & 50k’s), plus my current regular training here, (including road bike rides in 100+f), may be causing / have contributed.
I can still train hard, still get very heat-acclimated where I can handle our conditions, but occasionally have one of those days.
Any thoughts appreciated,
Scott
Hi Scott,
Thanks for your interesting question. Yes lots of desert, dry-air training over the years could cause EIB. Interestingly there is no literature on total-body hydration and EIB symptoms, that being said, anecdotally I do know some athletes with diagnosed EIB who do think their symptoms are worse when they are dehydrated.
I wrote an article for irunfar about EIB and other similar breathing conditions that we see in ultra runners that you might find interesting: https://www.irunfar.com/2018/04/take-my-breath-away-non-asthma-breathing-problems-in-endurance-running.html
Corrine
Corrine
Corrine, appreciate this article and noting cold and the long term effects of exercising in it as something that can damage the lungs. One question I have is in your opinion, how cold is too cold to exercise? I know -4 F is a guideline. BUT!!! At 50 now, growing up in michigan and truly enjoying winter sports, all my life, I am observing my friends who I played hockey with growing up, seem to be developing more respiratory/pulmonary problems, EIB, at an alarming number. I can’t say its age at this point because they have started having trouble with EIB for example since we started hitting 40. With temps not being that cold playing ice hockey, compared to outdoors sports, I point it to the intense efforts given in hockey. I think you described it accurately in giving work beyond one’s physiological capacity that damages the lungs when exposed to cold. I also think that giving that amount of effort and starting at a young age or in developing lungs may contribute to problems. Can you give any reason for this or have any studies, please share and last, if you had a temp you would say avoid going out in to ski, or hike or bike, without a mask what would it be. All the best.
Hi Heath, yes EIB is actually really common in hockey players, speed skaters, and even swimmers because it’s a combination of ventilated rapidly and inhaling irritant. That irritant for hockey players is actually thought to be the ice resurfacing agents, and for swimmers the chlorine. There’s currently no set temperature recommendation for when to put a mask on, and it would likely change based on the population (age, general health, etc). For going out in colder temperatures I would mostly pay attention to your effort level, with single digit temperatures, keeping your ventilation rate lower (easier effort). There is more and more research coming out trying to better look at the longterm effects of exercising in adverse environments, but a lot of it right now if using cautious self judgement.
Great article! Sure appreciate the insight.
Corrine, this is a really helpful article and gives me insight into what a doc diagnosed me as having this past summer, when I had respiratory distress after a summer of high-altitude training and then “gunky” raspy lungs, shortness of breath and inability to breath deeply during the nighttime of the Ouray 100 (high altitude cold/dry air). He said I was experiencing exercise-induced bronchial spasms gave me an inhaler to use prophylactically next time I’m training or racing like that; do you think albuterol will help the condition of EIB? Thanks for your info.
Sarah, I had no idea this happened last year! It’s scary when you don’t know what it is. We do see EIB develop in those long cold dry air (altitude is notorious for) during high attitude races like Leadville, The Bear (+dust), HardRock, etc. If it is EIB an inhaler should help manage symptoms when they arise, as it’s a bronchodilator. If it is exercise-induced laryngeal obstruction (EILO, formerly known as vocal-cord dysfunction) a bronchodilator won’t work, but it sounds like they have you on the right treatment plan. I wrote an article in 2018 for irunfar in greater detail about all these different breathing problems we see in ultra runners: https://www.irunfar.com/2018/04/take-my-breath-away-non-asthma-breathing-problems-in-endurance-running.html
Super helpful, thanks Corrine. Yes, my lungs were a big limiting factor for me last summer and I believe ultimately caused my DNF at Ouray after 26 hours because I couldn’t get the oxygen my system needed, so my pace slowed to a crawl. I was literally pausing every couple of steps to try to catch my breath, but it hurt to breathe in and I could hear & feel fluttery and raspy crud in my lungs. I was catastrophizing that it might be high-altitude pulmonary edema, which added to my stress, but doc said no, “just” bronchial spasms & constriction. I really need to manage these symptoms if I hope to ever succeed in a high-altitude long ultra. Really appreciate your med/sci articles.